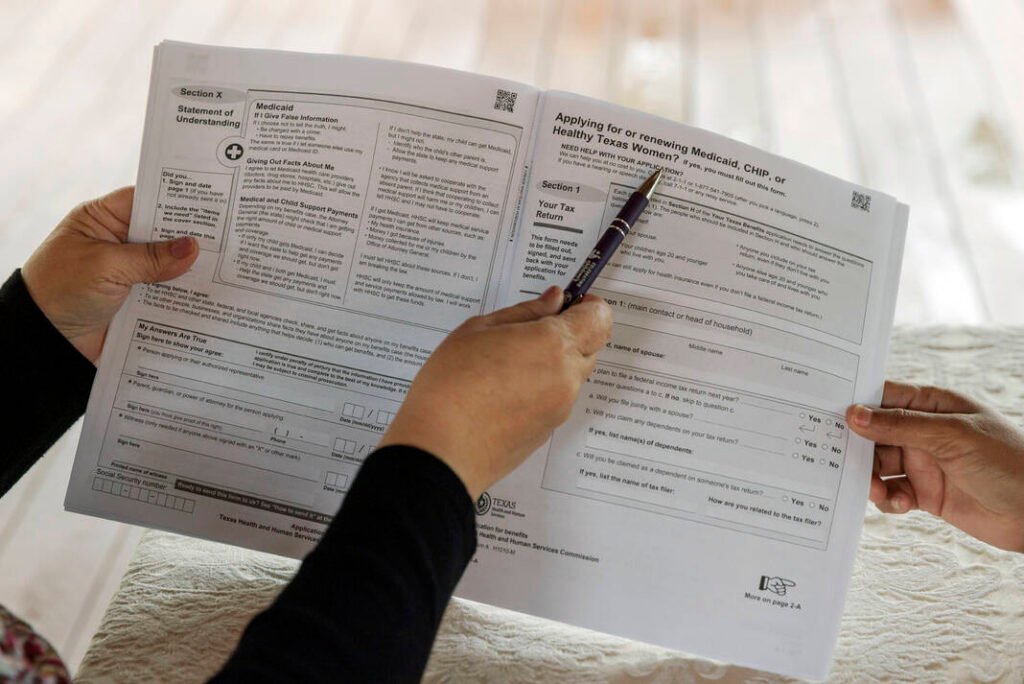
Understanding the Impact of the New Medicaid Requirement
On July 4, a significant piece of legislation known as the One Big, Beautiful Bill was passed, stirring concerns about its implications for millions of Americans relying on Medicaid. Experts estimate that this law may lead to cuts ranging from $800 billion to $1 trillion in funding for Medicaid, a vital healthcare program that has served as a lifeline for individuals in need of medical services for generations.
Key Changes in Medicaid Under the New Bill
Dr. Mark Kaswan, a political science professor at the University of Texas Rio Grande Valley, highlights two major changes stemming from this newly passed legislation. The first is a notable reduction in Medicaid funding aimed at achieving substantial cost savings. The second is the introduction of a Community Engagement Requirement, which will affect Medicaid eligibility for specific groups starting in 2027.
What is the Community Engagement Requirement?
Under the new regulations, individuals aged 19 to 64, who are neither pregnant nor disabled, and not enrolled in Medicare, will need to demonstrate active participation in work or community-related activities to retain their Medicaid eligibility. This requirement primarily targets those who have enrolled in Medicaid expansion under the Affordable Care Act (ACA).
To maintain eligibility, applicants must provide proof of completing at least 80 hours of work, volunteering, or community service monthly. They may also qualify by participating in educational programs or work programs, or by earning a monthly income equal to or exceeding the minimum wage for the same 80 hours. Any combination of these activities that totals 80 hours will be acceptable.
Individuals must meet these requirements for up to three months before applying for Medicaid. For current enrollees, compliance will be reassessed during eligibility reviews, potentially occurring more frequently based on state requirements.
States’ Role in Implementing the Requirement
States are mandated to verify whether individuals comply with the engagement requirement, using a standard set forth by the Secretary of Health and Human Services. They can rely on various sources, including payroll data and other available documentation. Notably, states cannot delegate compliance checks to Medicaid managed care entities.
If a state cannot confirm an individual’s compliance, it must issue a notice of noncompliance, giving the person 30 days to remedy the situation or explain why they are exempt from the requirement. Failure to respond or comply may lead to loss of coverage, although individuals must be informed of their rights to appeal and checked for other eligibility options before discontinuation.
The Broader Impact of the Changes
Despite the seemingly straightforward nature of these new requirements, Dr. Kaswan warns they could have negative consequences on communities, especially as a majority of Medicaid recipients are already engaged in the workforce. According to a KFF report, in 2023, 64% of adults under 65 who do not receive Social Security benefits were working, and the majority of those received Medicaid coverage.
The administrative hurdles created by these new requirements could deter people from applying for Medicaid. Drawing on examples from Georgia, which implemented similar work requirements in July 2023, Dr. Kaswan explains that a mere fraction of eligible residents enrolled, despite many being employed. This trend suggests that implementing such requirements could further reduce enrollment rates, particularly among vulnerable populations.
Comparison of Enrollment Rates
The challenges faced by Georgia residents are echoed in Arkansas’s experience when work requirements were enacted in 2018, leading to similar difficulties with system glitches and erroneous coverage cancellations.
In the Rio Grande Valley of Texas, where communities already experience high uninsured rates—ranging from 23.5% in Cameron County to 26.5% in Willacy County—these changes could prove devastating. According to the U.S. Census Bureau, as of July 2024, the region had a total of 357,586 Medicaid recipients, comprising nearly 25% of its population.
The Potential Consequences
Dr. Kaswan emphasizes that these legislative changes may ultimately counteract the original purpose of Medicaid, which is to ensure individuals receive necessary healthcare. Instead, they could lead to increased reliance on costly emergency room services—a less efficient and more expensive avenue for healthcare.
In light of this, preventive measures are crucial for effective and economical healthcare delivery, underscoring the need for accessible primary care.
Exceptions to the Community Engagement Requirement
While the new legislation sets forth strict compliance standards, several mandatory exceptions exist for groups such as:
- Individuals under 19 or over 65
- Pregnant women and postpartum individuals
- Those medically frail, blind, or disabled
- Parents or caregivers of children and disabled dependents
- Individuals undergoing substance abuse rehabilitation
- Participants in SNAP work programs
- Native Americans
- Incarcerated individuals
Temporary exemptions are also available for those facing short-term hardships, including hospitalization or natural disasters, and individuals living in areas with elevated unemployment rates. These exemptions will remain in effect until December 31, 2028, and the Centers for Medicare and Medicaid Services will receive $200 million in federal funding for the 2026 fiscal year to aid in implementation.
In conclusion, as this monumental legislation unfolds, understanding its implications is crucial for the millions reliant on Medicaid for their healthcare needs. With potential access hurdles looming, it’s imperative to stay informed and engaged in discussions surrounding these changes to safeguard the program’s future for those it serves.